Dr Tan Ngiap Chuan, who led the study and is the director of research at SHP, said the findings could prompt doctors to prioritise starting or adjusting medications with their patients. "We usually focus on other lifestyle factors first. We may switch the order now."

In addition to statins, a new class of injectables have emerged in recent years. They provide an alternative for patients “who are unable to achieve their targeted cholesterol levels, who are statin intolerant, or unable to adhere to regular therapies”, said Prof Tan.
These include the PCSK9 inhibitors (such as evolocumab and alirocumab), which are injected once every two weeks. There are also the small interfering RNA or siRNA, which requires subcutaneous injection only once every six months. These siRNA include inclisiran, which was recently approved by Singapore’s Health Sciences Authority and the US Food and Drug Administration, said Prof Tan. “The injectables can be used in combination with oral medicines.” Unfortunately, the commonly prescribed statins have received bad press on social media, said Prof Tan, even though they have been “proven to be effective in preventing heart attacks, strokes and death – even among low-risk patients”. It has led patients to develop “unfounded fears” for statin-associated side effects, he said. Here, Prof Tan tackles some of the common misconceptions patients have about statins:
MISCONCEPTION 1: Doctors prescribe statins as a catch-all

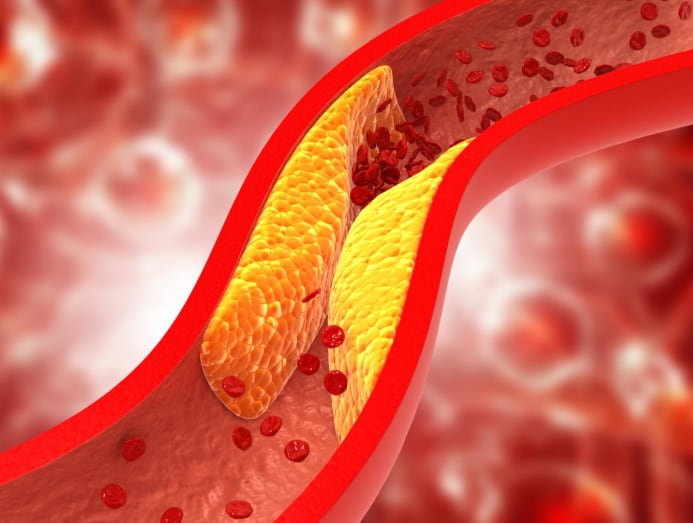
(Photo: iStock/wutwhanfoto)
Statins are widely used as they satisfy two crucial functions in disease management: Preventing the onset of disease before it begins; and reducing the severity or impact of a disease if it already has by “halting its progress and preventing recurrences”, said Prof Tan. “Certainly, patients who are at low risk for heart attack and stroke will benefit less from taking statins,” he said. But “among medical experts, there is little debate on whether statins work in high-risk patients”. Having said that, statins aren’t prescribed indiscriminately. According to Prof Tan, patients are usually started on a course only if they satisfy any of these criteria: Atherosclerotic cardiovascular disease. This means the patient has pre-existing blockages in the heart, brain or any arteries in the body’s circulatory system. Diabetes mellitus. Especially those who have been living with diabetes for more than 10 years. High LDL cholesterol level. Higher than 190mg/dL (4.9mmol/L). As prevention. These are patients with no established cardiovascular disease but have multiple risk factors that increase their chances of developing it in the future.
MISCONCEPTION 2: Once you start on statins, you have to be on them for life

This is true, though. The cholesterol-lowering benefits conferred by statins will only continue for as long as you take the medicine, said Prof Tan. “The cardio-protective effect is lost when the statins are stopped.” You would have considered to have discontinued your medication if you stopped for more than a year. Perhaps the more pertinent question is: What are the effects of being on statins in the long run? “Studies have shown that statins are safe and well tolerated. They have been used for more than 30 years to lower cholesterol. In fact, statins work best when you take them for a long time,” said Prof Tan. Look at it as insurance for a longer life and to prevent heart attacks and strokes, he added.
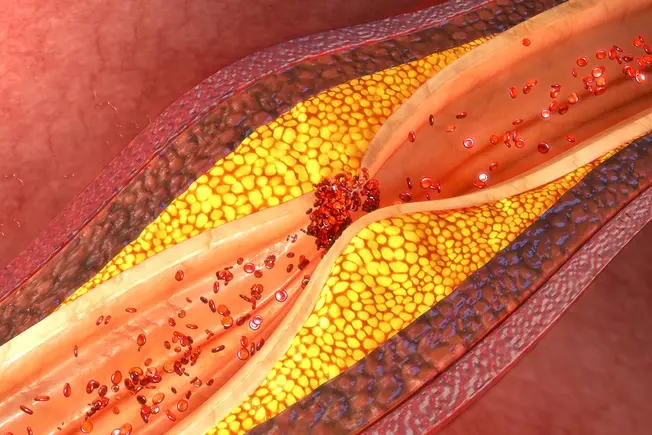
MISCONCEPTION 3: Statins cause diabetes

(Photo: iStock/hinnapong)

Source: CNA/bk Source link
Storvas C®
Kegunaan:
Menurunkan tahap kolesterol LDL
Mengurangkan risiko serangan jantung dan angin ahmar (strok)
Cara pengambilan:
1-4 biji 1 kali sehari selepas makan pada waktu malam
Kesan sampingan:
Kesan sampingan yang biasa:
Cirit-birit (sehingga 14.1%)
Sakit sendi (sehingga 11.7%)
Sakit otot (sehingga 8.4%)
Hidung tersumbat atau bersin (sehingga 8.3%)
Sila beritahu doktor jika kesan sampingan tersebut berterusan atau bertambah teruk.
Kesan sampingan yang serius tetapi jarang berlaku:
Reaksi alahan ubat (ruam, bengkak mulut atau mata, sesak nafas)
Sakit otot yang tidak dapat dijelaskan atau lemah
Peningkatan enzim hati
Pendarahan otak
Sila beritahu doktor dengan segera jika mengalami kesan sampingan yang serius.
Ini bukanlah senarai lengkap kesan-kesan sampingan yang boleh berlaku. Sila hubungi doktor atau pegawai farmasi untuk maklumat lanjut.
Penggunaan jika mengandung:
Kategori X: Elakkan penggunaan – kajian telah menunjukkan kesan mudarat dan boleh menyebabkan kecacatan kepada janin
Penggunaan jika menyusukan anak:
Elakkan penyusuan – terdapat risiko kesan mudarat kepada bayi
Kontraindikasi:
Sejarah reaksi alahan terhadap ubat ini atau bahan dalam ubat ini
Penyakit hati
Peningkatan enzim hati secara berterusan tanpa sebab yang diketahui
Sila huAtorvastatin 20 mg Film-coated Tablets – (emc) bungi doktor atau pegawai farmasi anda untuk maklumat lanjut
--------------------------------------------------------------------------
Brand:Storvas C® Usage:
Lowers LDL cholesterol levels
Reduces the risk of heart attack and stroke
How to take:
1-4 seeds 1 time a day after eating at night
Side effect:
Common side effects:
Diarrhea (up to 14.1%)
Joint pain (up to 11.7%)
Muscle pain (up to 8.4%)
Stuffy nose or sneezing (up to 8.3%)
Please tell your doctor if these side effects persist or worsen.
Serious but rare side effects:
Allergic drug reaction (rash, swelling of the mouth or eyes, shortness of breath)
Unexplained muscle pain or weakness
Increased liver enzymes
Brain hemorrhage
Please tell your doctor immediately if you experience any serious side effects.
This is not a complete list of possible side effects.
Please contact your doctor or pharmacist for more information.
Use if pregnant:
Category X: Avoid use – studies have shown harmful effects and may cause birth defects
Use if breastfeeding:
Avoid breastfeeding – there is a risk of harm to the baby
Contraindications:
History of allergic reactions to this drug or ingredients in this drug
Liver disease
Persistent elevation of liver enzymes for no known reason
Please contact your doctor or pharmacist for more informationJenama:
----------------------------------------------------------------------------
Description
Atorvastatin is a cholesterol-lowering medicine. It works by blocking the action of an enzyme responsible for the production of cholesterol in the body. Thus, it helps in reducing blood cholesterol levels. It also prevents the risk of heart problems.
Atorvastatin may cause common side effects such as headache, nausea, diarrhoea/constipation, indigestion, muscle pain, stuffy nose, etc. Consult your doctor if these symptoms persist for a long time or if they become severe. Atorvastatin can be taken with or without food as instructed by your doctor. Take it at the same time every day to maintain a constant level of this medicine in your body. Do not skip a dose or discontinue the treatment without consulting your doctor.Atorvastatin is not recommended if you are allergic to it, or have liver problems. Inform your doctor if you have diabetes as this medicine may affect your blood sugar control. This medicine is not recommended for use if you are pregnant or are breastfeeding.





No comments:
Post a Comment